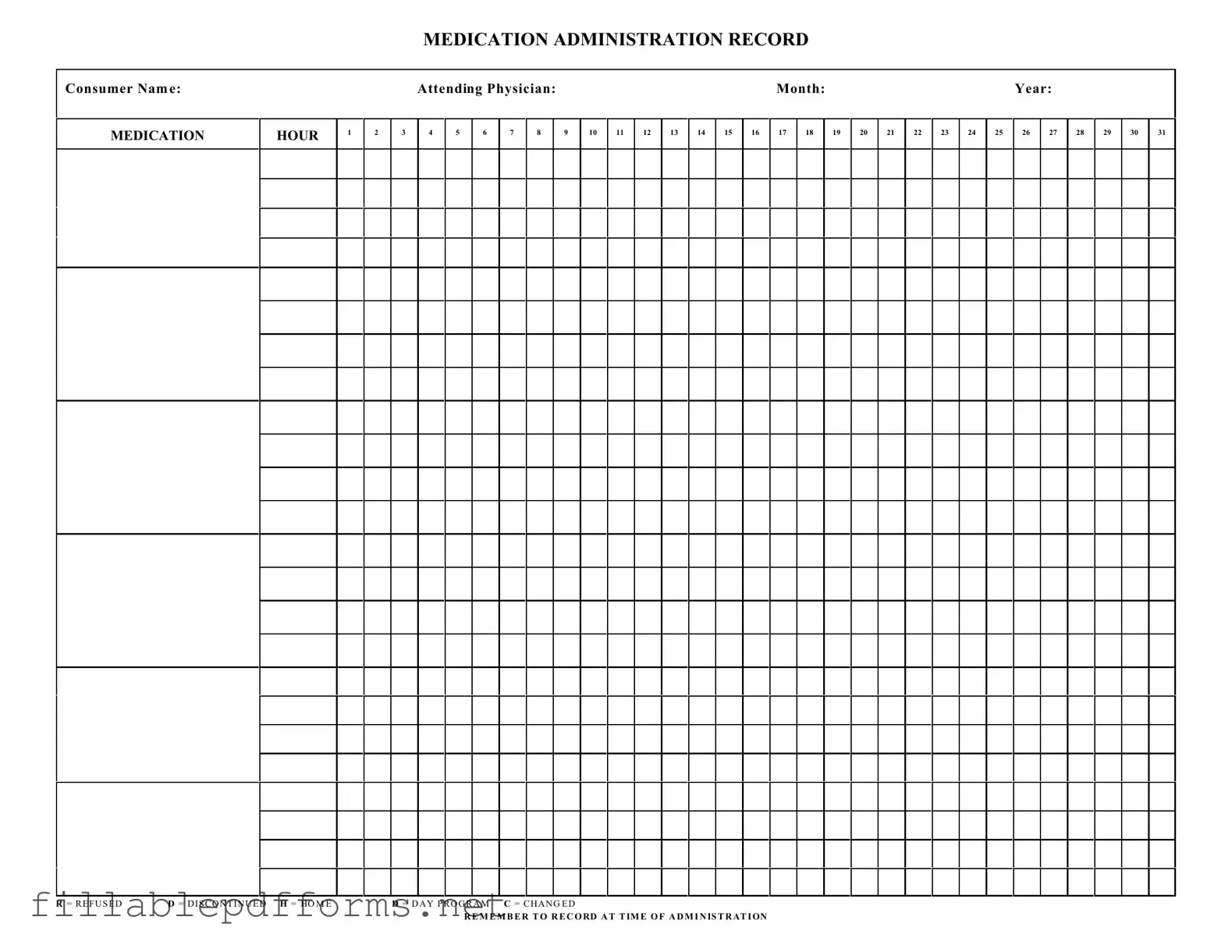
Medication Administration Record Sheet PDF Template
The Medication Administration Record Sheet is a vital tool used in healthcare settings to track the administration of medications to patients. This form ensures that all medications are documented accurately, allowing for effective communication among healthcare providers. By recording each dose and noting any refusals or changes, the form plays a crucial role in patient safety and care continuity.
Launch Editor Here
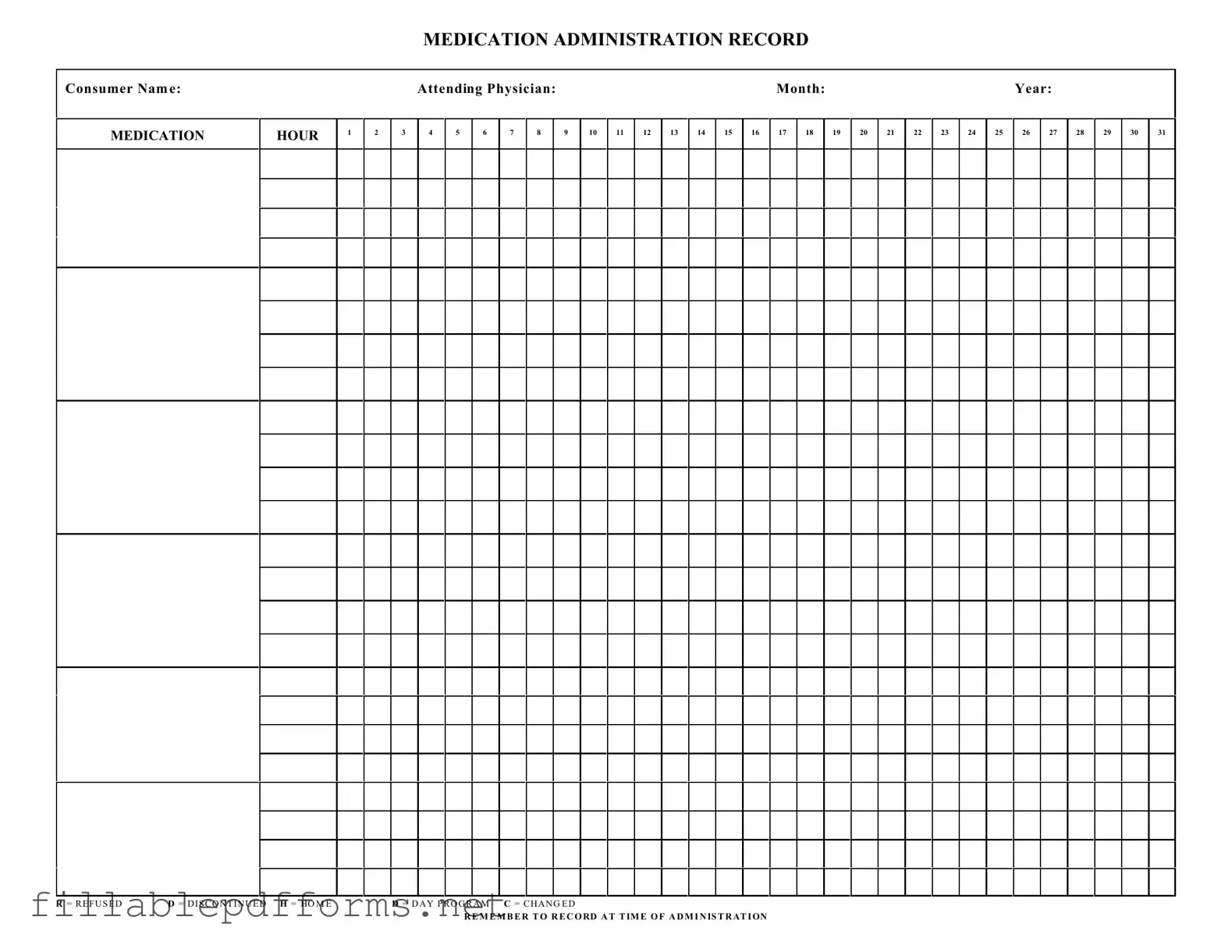
Medication Administration Record Sheet PDF Template
Launch Editor Here
Launch Editor Here
or
▼ Medication Administration Record Sheet PDF
Almost there — finish the form
Complete Medication Administration Record Sheet online fast — no printing, no scanning.