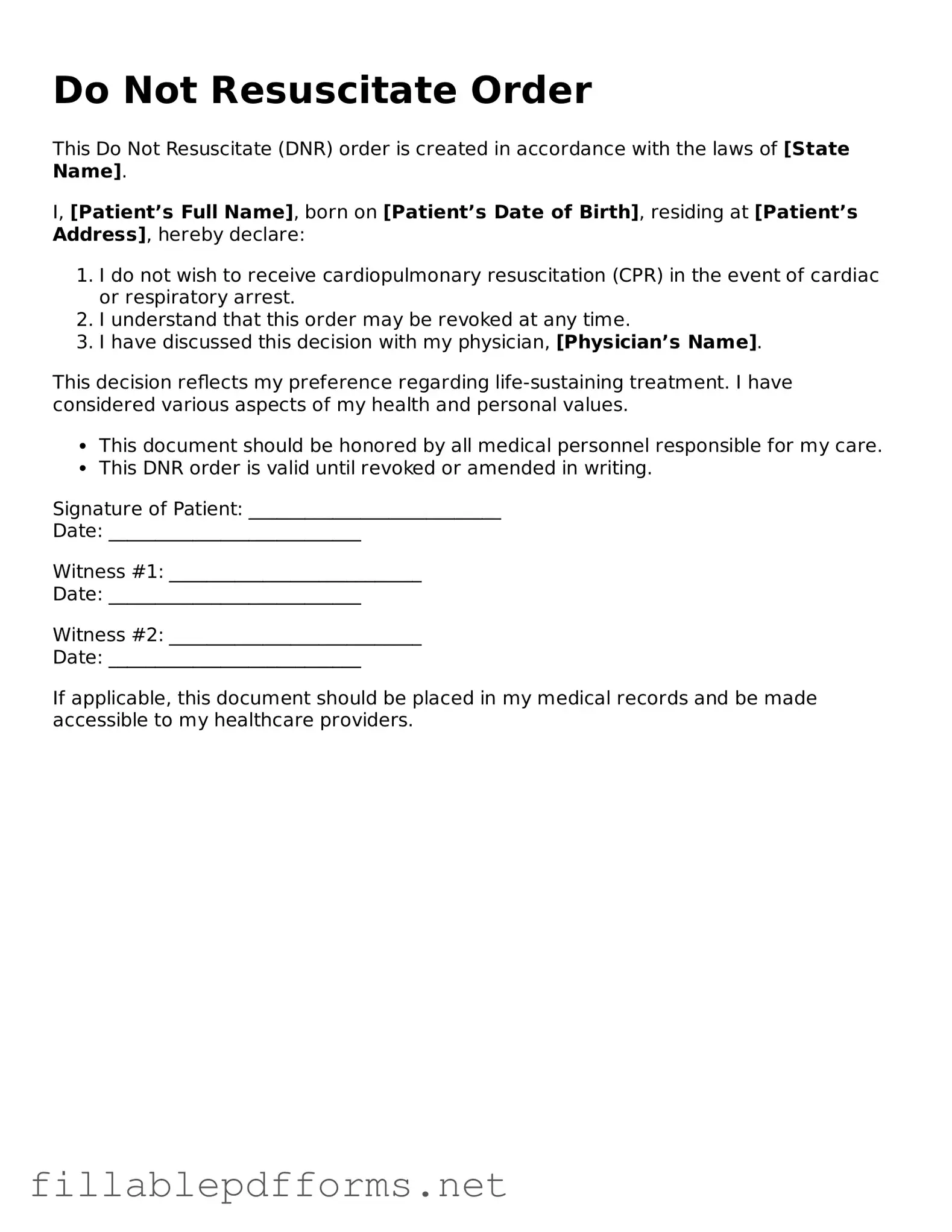
Blank Do Not Resuscitate Order Template
A Do Not Resuscitate (DNR) Order is a legal document that allows individuals to express their wishes regarding resuscitation efforts in the event of a medical emergency. This form ensures that healthcare providers respect a person's desire to avoid life-saving treatments that may not align with their values or goals. Understanding the implications of a DNR Order is crucial for anyone considering their end-of-life care options.
Launch Editor Here
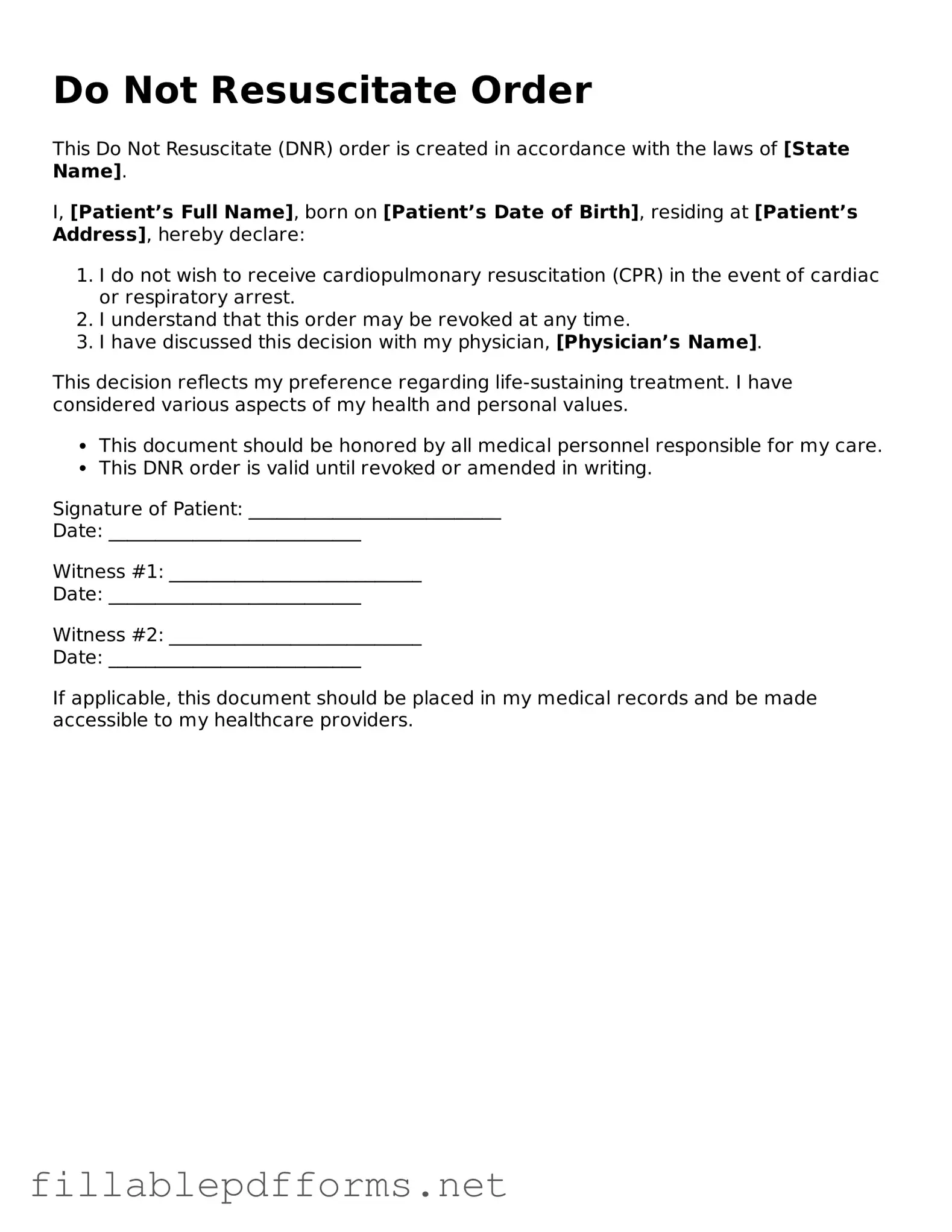
Blank Do Not Resuscitate Order Template
Launch Editor Here
Launch Editor Here
or
▼ Do Not Resuscitate Order PDF
Almost there — finish the form
Complete Do Not Resuscitate Order online fast — no printing, no scanning.